Canadian Health&Care Mall Experts Know How To Not Let Depression Rob You Of Life’s Joys
Those who suffer from depression are also mild, they know well some symptoms: they often feel exhausted, uninteresting, unable to turn on their days. The vital energy begins to disappear and, little by little, we are helpless at the touch of any impulse. Depression is not only a psychic discomfort: it is an imbalance that is heavily interfered with the overall health of those who suffer, which affects the vital functions most closely associated with well-being and psycho-physical health, starting with sleep, from appetite and sexual desire.
Depression definition by Canadian Health&Care Mall
Depression is a very common and well-known psychiatric disease. During the depressive state, patients feel hopeless and experience a sense of uselessness, inability and despair. The depressive state not only involves the mood and mind of the patient but also affects the body, alters the eating habits, sleeping, perceiving oneself, affective behaviors, and the behavior of an individual.

Depression causes the whole body to suffer. The efficiency of the immune system, as a rule, is heavily overwhelmed; it is not at all easier to fall ill in times of sadness and depression than in those of happiness. The consequence is a loss of confidence in oneself and in the future, everything seems gray and the slightest difficulty is able to send us to the rug. Yet depression, like many other discomforts, can also be read as a signal that comes to the effect of changing some of the crucial aspects of our existence, stubborn aspects and no longer functional to our evolution.
Depression is one of the five most common pathologies in the Western world and affects 12% of the population. The incidence of this disease in men and women is 1:2. Depression may develop even in pediatric and adolescent age, with an incidence of one child every 50 under 12 and a teen every 20. Particularly, adolescent depression affects mainly girls, probably due to hormonal and bodily changes occurring in puberty. Premenstrual depression (PMS) and postpartum depression represent other depressive states in the female sphere where the cause of the disease can be attributed to hormone variation.
Depression, however, also affects the elderly. In this category of patients, the symptoms associated with depressive disease are often attributed to a normal aging condition; this can cause a lack of diagnosis, resulting in worsening of the disease. Also, very often elderly people are reluctant to manifest feelings of sadness or despair and this makes the diagnosis of depression even more difficult.
In any case, whatever the cause of depression and the category of affected patients, it is necessary to intervene as early as possible with accurate diagnosis and appropriate pharmacological treatment to avoid chronic pathology. There are many types of depression that can be differentiated according to the type and severity of the symptoms and on the basis of their onset. Below, some of the most well-known depressive disorders are briefly explained by Canadian Health&Care Mall technicians.
Unipolar depression or major depression (MDD). This form of depression is the most serious of the various types of depressive disorders. It manifests itself with symptoms that prevent normal activities – such as working, studying, eating, sleeping – and preventing activities from happening. It seems that the major depression has family predispositions and seems to be hereditary.
Treatment is generally pharmacological and accompanied by psychotherapy. In very severe cases, electroconvulsive therapy (otherwise known as electroshock) could also be used.
Dysthymia. Dysthymia is a mood disorder with very similar symptoms to depression. These symptoms appear milder, but tend to persist for long periods (usually two years or more for adults and one year in children and adolescents). Treatment of this disorder is pharmacological and psychotherapeutic.
Bipolar disorders (manic-depressive disorders). Bipolar disorders are characterized by an alternation of depressive states and manic or hypomaniac states.
These psychiatric disorders are divided into:
- Type I bipolar disorder (characterized by manic-depressive episodes);
- Bipolar Type II Disorder (characterized by hypomania-depressive episodes);
- Cyclotymatic disorder or cyclotymy (a disorder with a minimum duration of two years and characterized by hypomania-depressive episodes).
The pharmacological treatment of this type of disorder involves the use of mood stabilizers (such as, for example, lithium) or an association of antidepressant and antipsychotic drugs.
Read the most popular recommendations offered by specialists: Getting Over Depression Until It Gets You
Causes of depression
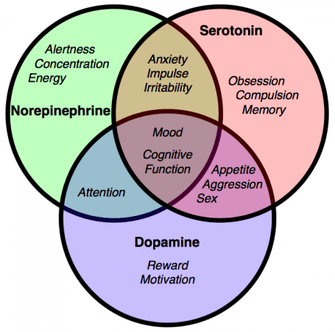 To date, it is believed that the cause of depression is due to the role played by certain types of neurotransmitters. These neurotransmitters are serotonin monoamine (or 5-HT), noradrenaline (or NA) and dopamine (or DA). To better understand the mechanism of action of these neurotransmitters, a brief premise on their physiology is indispensable. Serotonin, norepinephrine and dopamine are synthesized within monoaminergic neurons. Specifically, 5-HT is synthesized in serotonergic neurons, NA in noradrenergic neurons and DA in dopaminergic neurons.
To date, it is believed that the cause of depression is due to the role played by certain types of neurotransmitters. These neurotransmitters are serotonin monoamine (or 5-HT), noradrenaline (or NA) and dopamine (or DA). To better understand the mechanism of action of these neurotransmitters, a brief premise on their physiology is indispensable. Serotonin, norepinephrine and dopamine are synthesized within monoaminergic neurons. Specifically, 5-HT is synthesized in serotonergic neurons, NA in noradrenergic neurons and DA in dopaminergic neurons.
Once synthesized, the monoamines are stored in vesicles and released into the synaptic sphere (the space between the presynaptic and the postsynaptic nervous terminations) in response to certain stimuli. Once released into the synaptic space, the monoamines interact with their receptors on both the postsynaptic nervous termination membrane and the membrane of the presynaptic nerve ending. Such interaction results in a cascade of signals leading to a definite biological response.
After exposing their function, monoamines bind to receptors responsible for their reuptake (SERT for serotonin reuptake and NET for reuptake of noradrenaline) and are reported within presynaptic nerve termination. Once extracted, monoamines are metabolised by specific enzymes, monoamine oxidase (MAO) and catechol-O-methyl transferase (COMT). In fact, the exact cause of depression is not well known. In this regard, various assumptions have been made:
a) Monoaminergic hypothesis
According to this hypothesis, depression would be caused by a deficiency of serotonin, noradrenaline and dopamine. To support this theory is the fact that antidepressant drugs increase the transmission of these monoamines.
However, antidepressants alter the monoamine concentrations very quickly, but the therapeutic effect only takes weeks. Furthermore, there is no relationship between the power of the effect on extracellular concentration of monoamines and antidepressant efficacy; in other words, it is not said that a drug that can greatly increase the concentration of monoamine in the synaptic line has better antidepressant properties. Therefore, it is evident that the deficiency of serotonin, noradrenaline and dopamine can not be the only cause of depression.
b) Presumptive receptor hypothesis
This hypothesis states that depression is not simply caused by a monoamine deficiency, but also by an altered sensitivity of the postsynaptic receptors to these same neurotransmitters. The underlying concept of this theory is that in depressed patients, serotoninergic and noradrenergic postsynaptic receptors have become hypersensitive to their respective neurotransmitters as a result of their synaptic vascular dejection. Antidepressant drugs, therefore, would induce a hypoxicability of these same receptors and this would explain why the therapeutic effect is only established a few weeks after the start of the treatment.
c) Permissible hypothesis
This hypothesis highlights the importance of the mutual balance of serotonin and noradrenaline in the mood regulating processes. In fact, if the serotonin level is too low, noradrenergic regulation is lost and this can result in alterations in the levels of norepinephrine. Such alterations can lead to mania. If, however, the level of norepinephrine is lowered, serotoninergic regulation is lost, resulting in alteration of serotonin levels. This leads to the appearance of typical symptoms of depression.
d) Hormonal hypothesis
This hypothesis states that alteration of the hypothalamic-pituitary-adrenal axis (HPA) may be able to affect serotonin and noradrenaline levels released by the respective neurons, thus compromising their functioning. The various hypotheses thus agreed all agree that depression is due, directly or indirectly, to changes in serotonin and noradrenaline levels. As far as dopamine is concerned, although its role in the etiology of depression is still unclear, it is believed to be involved in the onset of the disease.
Although the monoaminergic hypothesis is insufficient to explain why depression develops, it still remains the most acclaimed hypothesis. The monoaminergic therapeutic approach is the most successful and, in fact, most antidepressant drugs act by increasing the serotoninergic and noradrenergic transmission.
Another common cause of depression that can massively affect individuals of various health condition across age and economical strata is something as trivial as the change of seasons. Transferring from one season to another might go smoothly for some people or for people at some point in their lives, and for others – or in another period of life – cause serious mood disorders.
The change of season causes various physiological effects on us, our lifestyle and our mood. Fatigue, depression, drowsiness, feeling of general malaise. These temporary disturbances make a long-awaited period, such as the beginning of spring, one of the most difficult of the year with regard to psycho-physical well-being. Seasonal change Seasonal affective disorder (SAD) is scientifically defined, leads to mood changes that have a cyclical pattern and affect each fall in the beginning and, at a lower percentage, at each spring start.
The most exposed categories to these disorders are the ‘weaker’ ones, such as children and the elderly; but not only, in fact, people who have particularly neglected or stressful lifestyles are greatly affected. Seasonal change is a critical moment for those who are already suffering from depression since the stresses our organism exerts have exacerbated existing disorders. The symptomatic picture is with sleep disturbances that occur with excessive drowsiness and excessive carbohydrates: they feel powerless and energetic, they are confused, anxious, and have difficulty in attention.
Although the cause of seasonal depressive affective disorder is unknown, research conducted so far suggests that the SAD is triggered by a melatonin cycle disorder, leading to an imbalance in the circadian cycle. It has been documented that when melatonin levels are abnormal (too high or too low), symptoms may be related to psychic disturbances. For example, recent studies have shown that melatonin levels are excessively high in people with manic disorders (subject to extreme mood swings) while they are too low in those who suffer from depression.
Canadian Health&Care Mall psychiatrists dish out 6 winning strategies against depression

Tip No 1. Seize this day. Living in the moment is the best way to avoid postponing actions and decisions, a very common tendency in depression but which is likely to leave us even more distant from the way life unfolds. In order to overcome sadness, it is imperative to take up the reins of one’s destiny. It does not matter if the mood and the circumstances come up short, instead of sitting, getting up, and acting.
Tip No 2. Take control over your life. It is your responsibility to win your depression firsthand. Therefore, whenever you face an adverse event, do not blame the case or the bad luck but begin to wonder what you have been doing. Only in this way will you be able to modify really harmful behaviors and behaviors that prevent you from the attainment of any goal, such as renunciation, distrust, sulking.
Tip No 3. Enjoy the benefits of detachment. The more we are bonded and dependent on material things, people, or convictions, we are more slaves to our possessive nature that binds well-being and sell out personal identity. In this way, we leave control over our happiness to external circumstances that are independent of our will. The opposite is also true: with the right detachment we return to give value to your inner freedom and the right to self-determination.
If you would like to read more about how to deal with the consequences on depression that has taken toll on your sexual health, please check out the following topics: Cialis Soft Tabs – Your Ally In Battling Erectile Dysfunction
Tip No 4. Cut short your complaining. Waking up to the positive things in your life is a winning strategy to dispel important energy you could use to bring about a positive change. The laments, then, do not like anyone and in times of greater discomfort you will focus on the shortcomings and failures, rejecting a chance to see your accomplishments and the proverbial blessings. In the long run, the risk is to engage in a prophecy that is self-proclaimed, where you and your close ones will expect only personal misfortunes and defeats from you.
Tip No 5. Set healthy boundaries. Learn to be the only person you are demanding about, but also learn to embrace your imperfections with grace. Do not hesitate to reject unacceptable advice, situations, conditions just because it will make you look nice. Just rely on your instincts and satisfy your genuine inner needs, go with your gut feeling and do not sell yourself out because of a false feeling of morality imposed from the outside. You will gain confidence and personality.
Tip No 6. Increase satisfaction factor. Focus exclusively on pleasing images and events. Remember the last time you felt fulfilled, happy and satisfied? Relive those very emotions: glowing eyes, a sprint in your walk, the feeling of empowerment. Hold this image of your success for several minutes, several times a day; gradually, this will boost your self-esteem.
Canadian Health&Care Pharmacy historical facts: antidepressants development
Antidepressants are a class of well-researched and widely used medications to treat mood disorders such as depression, major depression and bipolar disorder. Antidepressants In fact, these drugs are also used today in the treatment of neuropathic pain, obsessive-compulsive disorders, and smoking-disassembling therapy. To understand how antidepressants have been developed, and to better understand the meaning of their mechanism of action, it is helpful to know what depression is and what its possible causes are.
Before 1950 there were no antidepressant drugs as we mean today. The only therapies used in the treatment of depression were focused on the use of amphetamine stimulants or electro-convulsant therapy. However, the use of amphetamine drugs often proved to be ineffective, resulting in a single increase in patient activity and energy. Electroconvulsive therapy, on the other hand – though effective – terrorized patients because it caused pain.
The first antidepressant drugs were discovered in the late 1950s. Such drugs were tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (IMAOs). As has happened to many of the most important man-made discoveries, the antidepressant synthesis did not originate from the design but from the case. The founder of tricyclic antidepressants – imipramine – was discovered by Swiss psychiatrist Ronald Kuhn while looking for new chlorpromazine-like compounds for the treatment of schizophrenia. The second great discovery was that of monoamine oxidase inhibitors. Again, this discovery was done by chance by the development of isoniazid analogues (nicotinic acid hydrazide), a drug used in the treatment of tuberculosis.
The first analogue of isoniazide to be synthesized was the hyprinide. During the clinical trials of this derivative, there was considerable improvement in mood in patients with tuberculosis. However, hyprinidosis was found to be hepatotoxic to the therapeutic doses necessary to achieve both antituberculous action and antidepressant action.
The discovery of the antidepressant action of hyprionid, however, gave impetus to the search for new monoamine oxidase inhibitors. This impulse led to the synthesis of hydrazine derivatives and non-hydrazine derivatives with a lower toxicity than that induced by hyronazide.
However, due to the side effects that the first TCA and IMAO induced – especially at the cardiovascular level – the search for new drugs that could increase monoaminergic signal without causing such serious adverse effects was necessary. In the late 1960s, it was discovered that some antihistaminic drugs were able to selectively inhibit serotonin reuptake and were free of cardiotoxicity.
Since the importance of serotonin in depressive diseases was already clear with the use of TCAs and IMAOs, the purpose of pharmaceutical chemists was to identify and synthesize selective serotonin reuptake inhibitors (SSRIs) with the aim of obtain highly selective compounds for the serotonin reuptake conveyor but with fewer side effects – or at least with less serious side effects – than those induced by TCA and IMAO.
The first success in this field was achieved with the synthesis of zimeldine, a derivative of amitriptyline (a TCA). In fact, this molecule was able to selectively inhibit 5-HT reuptake with a minimal effect on noradrenaline reuptake and did not exhibit the typical side effects of TCA. Zimeldine was then withdrawn in the early 1980s as it favored the development of Guillain-Barré syndrome.
In any case, the success achieved with zimeldine gave the impetus for the development of new antidepressant drugs. This impulse led to the discovery of many new SSRIs and other antidepressant drugs, such as noradrenaline and serotonin reuptake inhibitors (NSRIs), in the late 1970s.
Antidepressant medication classes
As mentioned above, the development of antidepressant drugs had a significant impetus towards the end of the 1970s and throughout the 1980s. This led to the synthesis of new and numerous molecules. Below are the main classes of antidepressant medicines still used today.

Tricyclic antidepressants (TCA)
As stated above, these drugs were the first true antidepressants to be discovered. TCAs inhibit both serotonin and norepinephrine reuptake by binding to receptors for their reuptake within presynaptic nervous termination, SERT and NET. However, these medications cause many side effects, as they also inhibit other body systems. For this reason, TCAs are termed ‘dirty drugs’.
In particular, TCAs are able to:
- Block muscarinic receptors (anticholinergic action);
- Block α1-adrenergic receptors;
- Block H1 receptors (antihistaminic action);
- Block sodium channels at the heart and at the central nervous system level.
Amitriptyline, imipramine, clomipramine, nortriptyline, desipramine and amoxapine are part of this class of drugs.
Selective serotonin reuptake inhibitors (SSRs)
SSRIs bind selectively to SERT, thus inhibiting serotonin reuptake. Unlike TCAs, they do not block muscarinic, adrenergic and serotonergic receptors and, above all, they are not cardiotoxic.
Fluoxetine, fluvoxamine, citalopram, escitalopram, sertraline and paroxetine belong to this class of drugs.
Noradrenaline and serotonin reuptake inhibitors (NSRI)
As the name suggests, these drugs inhibit both serotonin and noradrenaline reuptake by binding to SERT and NET receptors. In a sense, TCAs can be considered the precursors of this class of antidepressants. However, NSRIs – unlike their tricyclic precursors – do not block other neuroreceptors and therefore have fewer side effects. Duloxetine and venlafaxine belong to this class of drugs.
Selective reuptake inhibitors of noradrenaline (NARI)
Selective recombination inhibitors of noradrenaline selectively bind to the NET receptor, thus enhancing the longer stay of the neurotransmitter in the synaptic spine. This class of drugs belongs to reboxetine.
Serotonergic transmission modulators (SARI)
Drugs belonging to this class exhibit their antidepressant action by enhancing serotoninergic transmission through antagonism towards the 5-HT2 receptors and through a weak inhibition of the reuptake of the same neurotransmitter. Trazodone and nefazodone are part of this category of drugs.
Noradrenergic and serotonergic transmission modulators (NASA)
This category of drugs plays its antidepressant action by antagonizing α2 adrenergic receptors and antagonizing 5-HT2 or 5-HT3 serotonin receptors. Mirtazapine belongs to this class of drugs.
Dopamine and noradrenaline reuptake inhibitors (DNRI)
These drugs selectively inhibit dopamine reuptake and – to a lesser extent – that of norepinephrine. They may also have a mild inhibition of serotonin reuptake. This category of drugs belongs to bupropion, a drug used – in addition to the treatment of major depression – also in smoking cessation therapy.
Monoamine oxidase inhibitors (IMAO)
As their name suggests, these drugs act by inhibiting particular types of enzymes, called monoamine oxidase and metabolites of monoamines. Two isoforms of MAOs, MAO-A and MAO-B are known. Drugs used in the treatment of depression are non-selective MAO inhibitors – such as phenelzine and tranylcypromine – and selective MAO-A inhibitors, such as moclobemide. Selective MAO-B inhibitors, however, are mainly used in Parkinson’s disease therapy.
Mood stabilizers
Mood stabilizers are used to treat bipolar disorder. They can have both acute and long-term effects. The most well-known mood stabilizer is definitely lithium carbonate.
Herbal therapy
Herbal therapy may also be used to treat mild to moderate depression. In particular, we refer to the treatment of depressive pathology with the hypericum, otherwise known as St. John’s wort. In fact, this plant is able to inhibit serotonin reuptake just like SSRIs, but is also able to increase the levels of norepinephrine, resulting in increased energy and responsiveness. Finally, the hypericum is also able to increase dopamine levels, thus promoting an increase in the sense of well-being.
Many treatments are available for the treatment of depression; In general, in order to obtain healing in a shorter time, the patient is subjected to cross-treatment, ie based on both the psychotherapeutic approach and the pharmacological approach. Clearly, to distract the disease, the patient who has affection must have the will of the will and the collaboration, trying to look at what surrounds him in a different perspective, better: in doing so, the patient can get positive results in more limited times.
As mentioned, depression is a heterogeneous and multifactorial pathological condition, so the choice of a drug instead of another, and of a specialist rather than another, essentially depends on the severity of the condition. Some people complain of a depression so mild that they do not even need drugs for complete healing; others, however, fall into such a deep depression that they can not come up again, either with psychiatrists or with antipsychotics.
Below are the classes of medicines most used in depression therapy, and some examples of drug-specific features; it is up to the physician to choose the active ingredient and the most suitable posology for the patient, depending on the severity of the illness, the health of the patient and his response to the treatment:
Tricyclic antidepressants: useful for the treatment of depression of medium and severe, possibly associated with physical illness. These drugs are not indicated to treat mild to severe acute depression. Still, tricyclics are very much used in depression therapy associated with appetite alteration, insomnia, hypersomnia and related disorders. Most often, the very first symptom of rehabilitation is the improvement of sleep quality, clearly altered by depression.
Amitriptyline (e.g. Laroxyl, Triptizol, Adepril): initially, the drug may be taken at dosage of 75 mg per day divided into multiple doses over 24 hours; the dose may increase up to 150-200 mg. For adolescents and elderly people with depression, the initial dose is 30-75 mg. The medication should preferably be taken before bedtime.
Imipramine (e.g. Imipra C FN, Tofranil): Initially, the drug should be taken at dosage of 75 mg per day divided into multiple doses. Dosages up to 150-200 mg can be increased; In some patients with depression, the dose of the drug may increase up to 300 mg per day. The maximum dose to take before bedtime is generally 150 mg. This dose should be reduced when administered to elderly patients.
Nortriptyline (e.g. Dominans, Noritren): At the beginning of antidepressant therapy, it is recommended to take a low dose of medication and gradually increase it to 75-100 mg per day, to be fractionated in multiple doses over 24 hours. For adolescents and elderly people with depression, a lower dose is recommended (30-50 mg per day).
These just described are just some of the many tricyclic drugs; among other things, they are mentioned: clomipramine, dosulepine, doxepine, trazodonel, fepramine.
At present, tricyclic drugs are less used in therapy due to their obvious side effects: vision alterations, anorgasmia, weight gain, hypertension, sexual difficulties, water retention, tachycardia.
Selective serotonin reuptake inhibitors: these drugs, second-generation antidepressants, replaced tricyclics in a short time, given the fewer side effects: these drugs, in fact, lack cholinergic action, implicated instead in the manifestation of the secondary effects of tricyclics. Selective serotonin reuptake inhibitors are not effective for severe forms of depression.
Fluoxetine (Prozac): Depending on severity of depression, it is recommended to take the drug at doses of 20-40 mg per day. Generally, during the first week of treatment, the drug causes nausea, a condition that tends to disappear in a short time. Continue the therapy for at least 3 weeks, unless otherwise indicated by the treating physician.
Citalopram (e.g. Seropram): Take a dose of 20-40 mg daily. The dose may be increased after a few weeks of therapy. Do not exceed 60 mg per day for adults and 40 mg per day for the elderly.
Sertraline (e.g. Zoloft, Sertralina, Tralisen): It is recommended to initiate therapy with an active dose of 50 mg / day. If necessary, increase the dose of 50 mg every 2-3 weeks. Do not exceed 200 mg per day. The maintenance dose is 50 mg daily.
Noradrenaline and dopamine reuptake inhibitors:
Bupropion (Wellbutrin): This is a drug used to treat mild to moderate depression; the active ingredient, unlike previous drugs, does not give drowsiness and interferes less with sexual desire. It is recommended to start treatment with 100 mg of active substance, to be taken by mouth twice a day. Maintenance dose: Take 75-100 mg of medication daily, increasing the dose, when needed, every 3 days (100 mg per os, three times a day). Do not exceed 450 mg per day divided into 4 doses. Therapy should be continued until symptoms are remedied or as prescribed by your doctor. The drug is widely used in smoking therapy.
Serotonin reuptake inhibitors and norepinephrine reuptake inhibitors:
Duloxetine (e.g. Xeristar, Yentreve, Ariclaim, Cymbalta): indicated for the treatment of major depression (in which the patient complains of severe mood depression for at least two consecutive weeks). It is recommended to take a dose of 40 mg, divided into two doses of 20 mg in 24 hours. In some cases, you can take two 30 mg doses each, without food.
Venlafaxine (e.g. Efexor): indicated for treating generalized depression and anxiety. Compared to tricyclic antidepressants, Venlafaxine does not produce typical antimuscarinic and sedative side effects. At the start of treatment, it is recommended to take 75 mg of active substance per day, preferably divided into two doses; continue for 3-4 weeks. If necessary, in this first period, you can increase the dose up to 150 mg (divided into two doses). In case of severe depression, increase the dose of 75 mg every 2-3 days. Do not exceed 375 mg per day.
Monoamino Oxidase Inhibitors (IMAOs): These drugs represent the last beach, when depression treatment with tricyclic drugs or SSRIs did not bring any real benefit to the depressed patient. These are second-choice drugs for the side effects they may generate. IMAOs are often available as a combination of several drugs, so as to enhance the final effect and reduce the time of treatment, so the likelihood of side effects decreases.
Fenelzine (e.g. Margyl): start therapy with 15 mg of medication three times a day. Maintenance dose: If necessary, increase dosage up to 60-90 mg daily. After getting the maximum benefit from the drug, it is recommended to gradually decrease the dose (15 mg per day and every other day) until the administration is complete.
Isocarboxazide (e.g. Marplan): Begin depression therapy by taking 10 mg of active substance twice a day. You can increase the dose of 10 mg every 2-4 days, up to 40 mg per day during the first week of therapy. Then, increase, if necessary, 20 mg every week (do not exceed 60 mg / day). Always split the dosage in 2-4 doses. Again in this case, after getting the maximum therapeutic response, gradually decrease the dose of the drug, to avoid the rebound effect. The maintenance dose is 40 mg per day divided into multiple doses. Consult your doctor.
Tranquipromine (e.g. Parmodalin): Compared to phenelzine and isocarboxazide, this drug is the most dangerous in terms of side effects, as well as being the most exciting. Indeed, the recommended dose for depression (10 mg twice daily in the first week, 30 mg daily in the second week, 10 mg per day for the maintenance dose) should not be given after 3 pm (gives insomnia because of hyper-excitability). This drug is contraindicated for the care of the baby’s depression.
It was a review done by Canadian Health&Care Mall experts canadianhealthcaremall.com on antidepressant types and on overcoming depression without pills. We suggested this second method as antidepressant take their toll on your body and are addictive. We recommend that you, under medical supervision, try improve your lifestyle and skip the need in taking antidepressants.


